Watch Luzaan Africa, a PHC worker, call out to you to join the AfroPHC for UHC Workshop on 10th December.
Category Archives: News
News
Join us on 10th Dec 2020

AfroPHC Statement
The African Forum for Primary Health Care (AfroPHC) came together in a three-day virtual workshop 4-7pm 9-11th September 2020, with 398 registrants from 28 African countries and ±100 participants per day. Each day involved an hour of moderated discussion between leaders of an illustrious list of organisations supporting AfroPHC, small breakout discussions involving participants and then feedback from groups and participants themselves. The workshop considered the following questions:
- What does the community expect from ambulatory PHC service delivery in Africa?
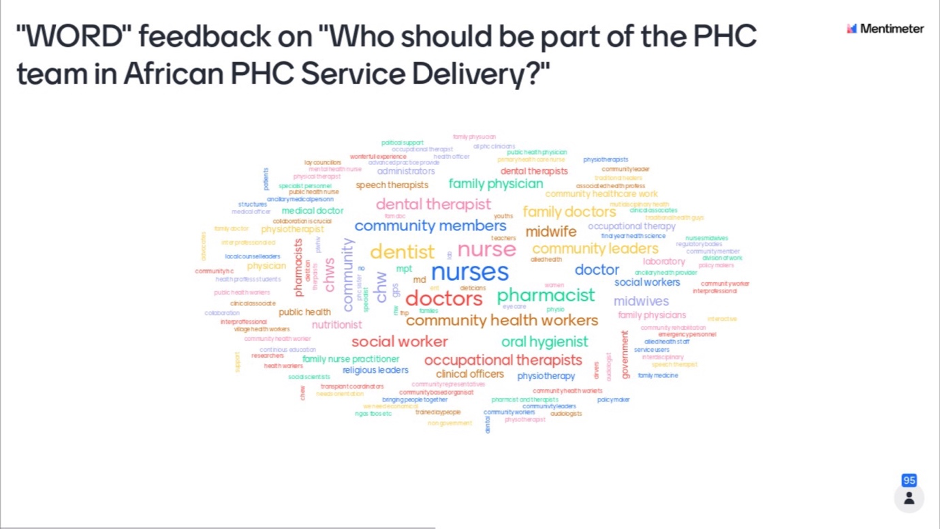
- Who should be part of the PHC team in African PHC Service?
- How should the PHC team work in ambulatory PHC service delivery in Africa?
- What support does the PHC team need in ambulatory PHC service delivery in Africa?
Participants felt report the workshop was outstanding for being highly interactive, informative, collaborative and productive. Next proposed steps include finalization of the statement, organizational development and clarification of specific objectives through additional workshops and expanding membership to include community voices.
“It was my first time to participate in such a brilliant platform” Joseph T. Kilasara
“The conference is one of its kind” Joyce Sibanda
The workshop emerged with the following statement:
“The African Forum for Primary Care (AfroPHC) consists of diverse multidisciplinary primary health care (PHC) workforce stakeholders from across Africa who share a vision for African PHC service delivery: It should be comprehensive, accessible, high quality, responsive to local needs, in partnership with communities and delivered by strong teamwork, training and supportive supervision.
Our key principles are:
- NATURE OF PHC: African PHC service delivery should be personal, holistic, comprehensive, continuous, integrated, high-quality, well-resourced, accessible, affordable, socially acceptable and empowering. It should be provided by skilled inter-disciplinary and intersectoral team-based care with public-private partnerships and referral support.
- PEOPLE-CENTRED PHC: African PHC service delivery should be responsive to the particular needs of communities in Africa and in partnership with them, linking and integrating facilities and communities.
- PHC HUMAN RESOURCES: Whilst nurses, midwives, clinical officers, family doctors and community health workers are all core to integrated PHC service delivery in Africa we believe all healthcare professionals (including mental health, rehabilitation, oral health etc.) and other stakeholders (patients, administrative staff, community, traditional services, local leaders etc.) need to be part of the PHC team in an interprofessional team-based approach that balances curative with preventive care. Community healthcare workers should be treated and paid as professionals. Different models of PHC service delivery teams need to be explored across Africa based on and optimized with clear and defined human resource and population data, understanding of community needs and country resources.
- PHC CAPACITY DEVELOPMENT: We believe that training of all healthcare professionals for PHC service delivery should be intensified and all professionals should be trained inter-professionally in different levels of comprehensive family and community care rather than just in narrow fragmented task-shifting. Health systems must ensure that all team members are well-trained in the principles of family medicine and PHC so as to deliver high quality bio-psycho-social-spiritual personal healthcare and be able to practice to a scope that is most efficient for each country.
- PHC TEAMWORK: We expect coordinated, collaborative and consultative interprofessional teamwork between us as an integrated PHC service delivery team with all team members demonstrating and supporting each other in skills of leadership and accountability. This should be supported by mandated interprofessional education, especially in undergraduate, basic training and continuing professional development.
- INCLUSIVE PHC LEADERSHIP: We will grow to be inclusive of all Anglophone, Francophone and Lusophone countries in Africa and provide good leadership as advocates – engaging politicians, community and PHC workers in a mix of collaboration, community engagement, training, research and guideline development.
- PHC ADVOCACY: We, as AfroPHC, see our way forward as building an Africa-specific, inter-disciplinary and inter-sectoral collaborative network for advocacy of PHC and UHC. We will advocate for:
- PHC teamwork to be prioritized with political and financial support and policies, education and training, infrastructure, community support, public-private partnerships, stronger supervision and teambuilding.
- Sufficient financial commitment to PHC, including encouraging community health insurance schemes; good management and effective leadership including effective communication; availability of medicines, equipment, diagnostics etc.; effective referral and transport systems and use of information and communication technologies.
- Availability of and incentives for a skilled and empowered PHC workforce to make a difference with the care needed in each community, especially in rural settings
- Interprofessional training-education and basic qualifications as well as ongoing health education, including team functioning, knowledge and practices, to provide quality care and training.
- Research and data collection as an integral part of PHC, including standardized human resource data
- A “health in all policies” framework for health promotion in the community.
Declaração AfroPHC
O Fórum Africano de Atenção Primária à Saúde (AfroPHC) reuniu-se em um workshop virtual de três dias das 16h às 19h, 9-11 de setembro de 2020, com 398 inscritos de 28 países africanos e ± 100 participantes por dia. Cada dia envolveu uma hora de discussão moderada entre os líderes de uma ilustre lista de organizações que apóiam o AfroPHC, pequenas discussões abertas envolvendo os participantes e então o feedback dos grupos e dos próprios participantes. O workshop considerou as seguintes questões:
• O que a comunidade espera da prestação de serviços ambulatoriais de APS na África?
• Quem deve fazer parte da equipe de APS no Serviço Africano de APS?
• Como a equipe de APS deve trabalhar na prestação de serviços ambulatoriais de APS na África?
• De que apoio a equipe de APS precisa para a prestação de serviços ambulatoriais de APS na África?
Os participantes sentiram que o relatório do workshop foi excelente por ser altamente interativo, informativo, colaborativo e produtivo. As próximas etapas propostas incluem a finalização da declaração, o desenvolvimento organizacional e o esclarecimento de objetivos específicos por meio de workshops adicionais e expansão do quadro de membros para incluir vozes da comunidade.
“Foi a primeira vez que participei de uma plataforma tão brilhante” Joseph T. Kilasara
“A conferência é única em seu tipo” Joyce Sibanda
O workshop surgiu com a seguinte afirmação:
“O Fórum Africano de Atenção Primária (AfroPHC) consiste em diversas partes interessadas multidisciplinares de atenção primária à saúde (APS) de toda a África que compartilham uma visão para a prestação de serviços de APS africana: Deve ser abrangente, acessível, de alta qualidade, responsivo às necessidades locais, em parceria com as comunidades e proporcionado por um forte trabalho em equipe, treinamento e supervisão de apoio.
Nossos princípios-chave são:
- NATUREZA DA APS: A prestação de serviços da APS africana deve ser pessoal, holística, abrangente, contínua, integrada, de alta qualidade, com bons recursos, acessível, acessível, socialmente aceitável e capacitadora. Deve ser fornecido por meio de cuidados qualificados, interdisciplinares e intersetoriais, com parcerias público-privadas e apoio de referência.
- APS CENTRADA NA PESSOA: A prestação de serviços de APS africana deve responder às necessidades particulares das comunidades em África e em parceria com elas, ligando e integrando instalações e comunidades.
- RECURSOS HUMANOS DE APS: Embora enfermeiras, parteiras, funcionários clínicos, médicos de família e trabalhadores comunitários de saúde sejam essenciais para a prestação de serviços de APS integrados na África, acreditamos que todos os profissionais de saúde (incluindo saúde mental, reabilitação, saúde bucal, etc.) e outras partes interessadas (pacientes, equipe administrativa, comunidade, serviços tradicionais, líderes locais, etc.) precisam fazer parte da equipe de APS em uma abordagem baseada em equipe interprofissional que equilibra cuidados curativos e preventivos. Os profissionais de saúde comunitários devem ser tratados e pagos como profissionais. Diferentes modelos de equipes de prestação de serviços de APS precisam ser explorados em toda a África com base e otimizados com recursos humanos e dados populacionais claros e definidos, compreensão das necessidades da comunidade e recursos do país.
- DESENVOLVIMENTO DA CAPACIDADE DE APS: Acreditamos que o treinamento de todos os profissionais de saúde para a prestação de serviços de APS deve ser intensificado e todos os profissionais devem ser treinados interprofissionalmente em diferentes níveis de atenção integral à família e à comunidade, ao invés de apenas em trocas estreitas e fragmentadas de tarefas. Os sistemas de saúde devem garantir que todos os membros da equipe sejam bem treinados nos princípios da medicina de família e da APS, de modo a oferecer cuidados de saúde pessoais bio-psico-sociais-espirituais de alta qualidade e serem capazes de praticar a prática de forma mais eficiente para cada país .
- TRABALHO EM EQUIPE DE APS: Esperamos um trabalho em equipe interprofissional coordenado, colaborativo e consultivo entre nós como uma equipe integrada de prestação de serviços de APS, com todos os membros da equipe demonstrando e apoiando uns aos outros em habilidades de liderança e responsabilidade. Isso deve ser apoiado por educação interprofissional obrigatória, especialmente na graduação, treinamento básico e desenvolvimento profissional contínuo.
- LIDERANÇA DE APS INCLUSIVA: Cresceremos para incluir todos os países anglófonos, francófonos e lusófonos na África e oferecer uma boa liderança como defensores – envolvendo políticos, comunidade e trabalhadores de APS em uma mistura de colaboração, envolvimento da comunidade, treinamento, pesquisa e desenvolvimento de diretrizes.
- DEFESA DE APS: Nós, como AfroPHC, vemos nosso caminho adiante como a construção de uma rede colaborativa interdisciplinar e intersetorial específica para a África para a defesa de CPS e cobertura universal de saúde. Vamos defender:
- O trabalho em equipe da APS deve ser priorizado com apoio político e financeiro e políticas, educação e treinamento, infraestrutura, apoio comunitário, parcerias público-privadas, supervisão mais forte e formação de equipes.
- Compromisso financeiro suficiente para a APS, incluindo o incentivo a esquemas de seguro saúde comunitário; boa gestão e liderança eficaz, incluindo comunicação eficaz; disponibilidade de medicamentos, equipamentos, diagnósticos etc .; sistemas eficazes de encaminhamento e transporte e uso de tecnologias de informação e comunicação.
- Disponibilidade e incentivos para uma força de trabalho qualificada e capacitada na APS para fazer a diferença com os cuidados necessários em cada comunidade, especialmente em ambientes rurais
- Formação interprofissional-educação e qualificações básicas, bem como educação permanente em saúde, incluindo o funcionamento da equipe, conhecimentos e práticas, para fornecer atendimento e treinamento de qualidade.
- Pesquisa e coleta de dados como parte integrante da APS, incluindo dados padronizados de recursos humanos
- Uma estrutura de “saúde em todas as políticas” para a promoção da saúde na comunidade.
Déclaration AfroPHC
Le Forum africain pour les soins de santé primaires (AfroPHC) s’est réuni dans un atelier virtuel de trois jours de 16h à 19h du 9 au 11 septembre 2020, avec 398 inscrits de 28 pays africains et ± 100 participants par jour. Chaque jour comportait une heure de discussion modérée entre les dirigeants d’une illustre liste d’organisations soutenant l’AfroPHC, de petites discussions en petits groupes impliquant les participants, puis les commentaires des groupes et des participants eux-mêmes. L’atelier a examiné les questions suivantes:
• Qu’attend la communauté de la prestation de services ambulatoires de SSP en Afrique?
• Qui devrait faire partie de l’équipe SSP dans le service SSP en Afrique?
• Comment l’équipe SSP devrait-elle travailler dans la prestation de services ambulatoires de SSP en Afrique?
• De quel soutien l’équipe SSP a-t-elle besoin pour la prestation de services ambulatoires de SSP en Afrique?
Les participants ont estimé que l’atelier était exceptionnel pour sa grande interactivité, ses informations, sa collaboration et sa productivité. Les prochaines étapes proposées comprennent la finalisation de la déclaration, le développement organisationnel et la clarification des objectifs spécifiques par le biais d’ateliers supplémentaires et l’élargissement du nombre de membres pour inclure les voix de la communauté.
«C’était la première fois que je participais à une plateforme aussi brillante» Joseph T. Kilasara
«La conférence est unique en son genre» Joyce Sibanda
L’atelier a émergé avec la déclaration suivante:
«Le Forum africain pour les soins primaires (AfroPHC) est composé de divers acteurs multidisciplinaires du personnel des soins de santé primaires (SSP) de toute l’Afrique qui partagent une vision de la prestation de services de SSP en Afrique: il doit être complet, accessible, de haute qualité, sensible aux besoins locaux, en partenariat avec les communautés et assuré par un solide travail d’équipe, une formation et une supervision de soutien.
Nos principes clés sont:
- NATURE DES SSP: La prestation de services de SSP en Afrique doit être personnelle, holistique, complète, continue, intégrée, de haute qualité, bien dotée en ressources, accessible, abordable, socialement acceptable et responsabilisante. Il doit être assuré par des soins en équipe interdisciplinaires et intersectoriels qualifiés avec des partenariats public-privé et un soutien à l’orientation.
- SSP CENTRÉS SUR LES PERSONNES: La prestation de services de SSP en Afrique doit être adaptée aux besoins particuliers des communautés en Afrique et en partenariat avec elles, reliant et intégrant les installations et les communautés.
- RESSOURCES HUMAINES DE SSP: Alors que les infirmières, les sages-femmes, les cliniciens, les médecins de famille et les agents de santé communautaires sont tous au cœur de la prestation intégrée de services de SSP en Afrique, nous croyons que tous les professionnels de la santé (y compris la santé mentale, la réadaptation, la santé bucco-dentaire, etc.) et d’autres parties prenantes (patients, personnel administratif, communauté, services traditionnels, dirigeants locaux, etc.) doivent faire partie de l’équipe de soins de santé primaires dans une approche d’équipe interprofessionnelle qui équilibre les soins curatifs et préventifs. Les agents de santé communautaires devraient être traités et payés comme des professionnels. Différents modèles d’équipes de prestation de services de SSP doivent être explorés à travers l’Afrique sur la base et optimisés avec des données claires et définies sur les ressources humaines et la population, la compréhension des besoins de la communauté et des ressources nationales.
- DÉVELOPPEMENT DES CAPACITÉS DE SSP: Nous croyons que la formation de tous les professionnels de la santé pour la prestation de services de SSP devrait être intensifiée et que tous les professionnels devraient être formés de manière interprofessionnelle à différents niveaux de soins complets de la famille et de la communauté plutôt que simplement dans une répartition étroite et fragmentée des tâches. Les systèmes de santé doivent veiller à ce que tous les membres de l’équipe soient bien formés aux principes de la médecine familiale et des soins de santé primaires afin de fournir des soins de santé personnels bio-psycho-sociaux-spirituels de haute qualité et être en mesure de pratiquer dans le cadre le plus efficace pour chaque pays.
- TRAVAIL D’ÉQUIPE DE SSP: Nous nous attendons à un travail d’équipe interprofessionnel coordonné, collaboratif et consultatif entre nous en tant qu’équipe intégrée de prestation de services de SSP, tous les membres de l’équipe démontrant et se soutenant mutuellement en matière de leadership et de responsabilité. Cela devrait être soutenu par une formation interprofessionnelle obligatoire, en particulier au premier cycle, la formation de base et le développement professionnel continu.
- LEADERSHIP INCLUSIF DES SSP: Nous grandirons pour inclure tous les pays anglophones, francophones et lusophones d’Afrique et fournirons un bon leadership en tant que défenseurs – en engageant les politiciens, les communautés et les travailleurs des SSP dans un mélange de collaboration, d’engagement communautaire, de formation, de recherche et de lignes directrices développement.
- PLAIDOYER SUR LES SSP: En tant qu’AfroPHC, nous voyons notre voie à suivre comme la construction d’un réseau de collaboration interdisciplinaire et intersectorielle spécifique à l’Afrique pour le plaidoyer pour les SSP et la CSU. Nous plaiderons pour:
- une. Le travail d’équipe des SSP doit être priorisé avec un soutien politique et financier et des politiques, l’éducation et la formation, les infrastructures, le soutien communautaire, les partenariats public-privé, une supervision renforcée et le renforcement de l’esprit d’équipe.
- Un engagement financier suffisant en faveur des SSP, notamment en encourageant les régimes d’assurance maladie communautaire; bonne gestion et leadership efficace, y compris une communication efficace; disponibilité des médicaments, équipements, diagnostics, etc .; systèmes efficaces d’orientation et de transport et utilisation des technologies de l’information et de la communication.
- Disponibilité et incitation pour une main-d’œuvre de SSP qualifiée et habilitée à faire une différence avec les soins nécessaires dans chaque communauté, en particulier en milieu rural
ré. - Formation-éducation interprofessionnelle et qualifications de base ainsi que l’éducation sanitaire continue, y compris le fonctionnement de l’équipe, les connaissances et les pratiques, pour fournir des soins et une formation de qualité.
- Recherche et collecte de données en tant que partie intégrante des SSP, y compris des données normalisées sur les ressources humaines
- Un cadre «la santé dans toutes les politiques» pour la promotion de la santé dans la communauté.
اجتمع المنتدى الأفريقي للرعاية الصحية الأولية (AfroPHC) في ورشة عمل افتراضية لمدة ثلاثة أيام من 4 إلى 7 مساءً من 9 إلى 11 سبتمبر 2020 ، مع 398 مسجلاً من 28 دولة أفريقية و ± 100 مشارك يوميًا. تضمن كل يوم نقاشًا خاضعًا للإشراف لمدة ساعة بين قادة قائمة بارزة من المنظمات التي تدعم AfroPHC ، ومناقشات فرعية صغيرة تضم المشاركين ثم ردود الفعل من المجموعات والمشاركين أنفسهم. تناولت الورشة الأسئلة التالية:
ماذا يتوقع المجتمع من تقديم خدمات الرعاية الصحية الأولية المتنقلة في أفريقيا؟
من يجب أن يكون جزءًا من فريق الرعاية الصحية الأولية في خدمة الرعاية الصحية الأولية الأفريقية؟
كيف يجب أن يعمل فريق الرعاية الصحية الأولية في تقديم خدمات الرعاية الصحية الأولية المتنقلة في إفريقيا؟
ما هو الدعم الذي يحتاجه فريق الرعاية الصحية الأولية في تقديم خدمات الرعاية الصحية الأولية المتنقلة في إفريقيا؟
شعر المشاركون أن ورشة العمل كانت رائعة لكونها تفاعلية وغنية بالمعلومات وتعاونية ومنتجة. تشمل الخطوات المقترحة التالية الانتهاء من البيان ، والتطوير التنظيمي وتوضيح أهداف محددة من خلال ورش عمل إضافية وتوسيع العضوية لتشمل أصوات المجتمع.
“كانت المرة الأولى التي أشارك فيها في مثل هذه المنصة الرائعة” جوزيف تي كيلاسارا
“المؤتمر فريد من نوعه” جويس سيباندا
خرجت الورشة بالبيان التالي:
“يتكون المنتدى الأفريقي للرعاية الأولية (AfroPHC) من أصحاب المصلحة المتنوعين في مجال الرعاية الصحية الأولية (PHC) من جميع أنحاء إفريقيا الذين يتشاركون رؤية لتقديم خدمات الرعاية الصحية الأولية في إفريقيا: يجب أن يكون شاملاً ، ويمكن الوصول إليه ، وعالي الجودة ، ومستجيب للاحتياجات المحلية ، بالشراكة مع المجتمعات ويتم تقديمها من خلال العمل الجماعي القوي والتدريب والإشراف الداعم.
مبادئنا الرئيسية هي:
طبيعة الرعاية الصحية الأولية: يجب أن يكون تقديم خدمات الرعاية الصحية الأولية في إفريقيا شخصيًا وشاملاً ومستمرًا ومتكاملًا وعالي الجودة ومزود بموارد جيدة ويمكن الوصول إليه وبأسعار معقولة ومقبول اجتماعيًا وممكّنًا. يجب أن يتم توفيرها من خلال رعاية ماهرة متعددة التخصصات ومشتركة بين القطاعات قائمة على الفريق مع شراكات بين القطاعين العام والخاص ودعم الإحالة.
الرعاية الصحية الأولية التي تركز على الناس: يجب أن يكون تقديم خدمات الرعاية الصحية الأولية في إفريقيا مستجيبًا للاحتياجات الخاصة للمجتمعات في إفريقيا وبالشراكة معها ، وربط المرافق والمجتمعات ودمجها.
الموارد البشرية للرعاية الصحية الأولية: في حين أن الممرضات والقابلات والمسؤولين السريريين وأطباء الأسرة والعاملين في صحة المجتمع هم جميعًا أساسيون لتقديم خدمات الرعاية الصحية الأولية المتكاملة في إفريقيا ، فإننا نعتقد أن جميع المتخصصين في الرعاية الصحية (بما في ذلك الصحة العقلية وإعادة التأهيل وصحة الفم وما إلى ذلك) وأصحاب المصلحة الآخرين (المرضى ، الموظفون الإداريون ، المجتمع ، الخدمات التقليدية ، القادة المحليون ، إلخ) يجب أن يكونوا جزءًا من فريق الرعاية الصحية الأولية في نهج فريق مهني قائم على الفريق الذي يوازن بين العلاج والرعاية الوقائية. يجب معاملة العاملين في مجال الرعاية الصحية المجتمعية ودفع أجورهم كمحترفين. يجب استكشاف نماذج مختلفة من فرق تقديم خدمات الرعاية الصحية الأولية في جميع أنحاء إفريقيا بناءً على بيانات الموارد البشرية والسكان الواضحة والمحددة وتحسينها ، وفهم احتياجات المجتمع وموارد الدولة.
تنمية قدرات الرعاية الصحية الأولية: نحن نؤمن بضرورة تكثيف تدريب جميع المتخصصين في الرعاية الصحية على تقديم خدمات الرعاية الصحية الأولية ، كما يجب تدريب جميع المهنيين بين المهنيين في مستويات مختلفة من الرعاية الأسرية والمجتمعية الشاملة بدلاً من مجرد تحويل المهام الضيقة والمجزأة. يجب أن تضمن النظم الصحية أن جميع أعضاء الفريق مدربون تدريباً جيداً على مبادئ طب الأسرة والرعاية الصحية الأولية من أجل تقديم رعاية صحية شخصية بيولوجية ونفسية واجتماعية وروحية عالية الجودة والقدرة على الممارسة في نطاق أكثر كفاءة لكل بلد .
فريق عمل الرعاية الصحية الأولية: نتوقع عمل جماعي مهني منسق وتعاوني واستشاري بيننا كفريق متكامل لتقديم خدمات الرعاية الصحية الأولية مع قيام جميع أعضاء الفريق بإظهار ودعم بعضهم البعض في مهارات القيادة والمساءلة. يجب أن يتم دعم ذلك من خلال التعليم الإلزامي بين المهنيين ، وخاصة في المرحلة الجامعية والتدريب الأساسي والتطوير المهني المستمر.
قيادة شاملة للرعاية الصحية الأولية: سننمو لنصبح شاملين لجميع البلدان الناطقة بالإنجليزية والفرانكوفونية واللوسوفونية في إفريقيا ونوفر قيادة جيدة كمدافعين – إشراك السياسيين والعاملين في المجتمع والرعاية الصحية الأولية في مزيج من التعاون والمشاركة المجتمعية والتدريب والبحث وتطوير المبادئ التوجيهية.
مناصرة الرعاية الصحية الأولية: نحن ، بصفتنا AfroPHC ، نرى طريقنا إلى الأمام من خلال بناء شبكة تعاونية خاصة بأفريقيا ومتعددة التخصصات وبين القطاعات لمناصرة الرعاية الصحية الأولية والتغطية الصحية الشاملة. سوف ندعو إلى:
يجب إعطاء الأولوية للعمل الجماعي للرعاية الصحية الأولية مع الدعم السياسي والمالي والسياسات والتعليم والتدريب والبنية التحتية والدعم المجتمعي والشراكات بين القطاعين العام والخاص وإشراف أقوى وبناء الفريق.
الالتزام المالي الكافي للرعاية الصحية الأولية ، بما في ذلك تشجيع خطط التأمين الصحي المجتمعي ؛ الإدارة الجيدة والقيادة الفعالة بما في ذلك الاتصال الفعال ؛ توافر الأدوية والمعدات ووسائل التشخيص وما إلى ذلك ؛ إحالة فعالة أ
AfroPHC: An Ally Improving PHC
AfroPHC is now an Ally Improving PHC

Dear friends,
Two years ago, at the Global Conference on Primary Health Care (PHC) in Astana, world leaders committed to strengthening PHC as the cornerstone of resilient health systems as the most effective pathway toward health for all. Now, the COVID-19 pandemic has made acting on those commitments more urgent than ever.
On today’s second anniversary of the Declaration of Astana, we are thrilled to announce the launch of the Allies Improving PHC, 29 diverse organizations committed to advancing PHC on the road to health for all. This community is joining together across regions and issue areas to call for collective action on improving PHC as the most effective way to meet the majority of health needs in times of crisis and calm. If your organization is committed to PHC and interested in becoming an Ally, we hope you will reach out through this survey.
We are excited to kick off #StrongerwithPHC, a virtual campaign to amplify and remind the global community of the promise of Astana. To amplify this critical call for stronger PHC for all, we hope you will join in online using this social toolkit, which includes content to promote, graphics to share and handles to follow throughout this week (26-30 October).
We are also delighted to share a commentary in BMJ Opinion – co-authored by the PHCPI Steering Committee Members – which highlights the commitments made at Astana and the importance of redoubling our efforts to improve PHC as we continue to contend with COVID-19.
We must strengthen PHC as the cornerstone of effective, equitable health systems as countries recover from the pandemic and beyond. Today, let us be reminded that we are #StrongerwithPHC, and that together, we can make #HealthforAll a reality.
Sincerely,

Beth Tritter
Executive Director
Primary Health Care Performance Initiative
Report on AfroPHC Workshop 9-11 Sept 2020
AfroPHC Workshop Report

DAY 1
The first session 4-7pm Central African time 9th September was moderated by Champion Nyoni. Participants were introduced to Mentimeter to provide feedback. There were over 100 participants from a number of countries in Africa (South Africa, Kenya, Nigeria, Uganda, Malawi, Sudan, South Sudan, Tanzania) as well as globally (USA, Belgium, Germany, Lebanon, Argentina and The Netherlands. Participants felt overwhelmingly excited about the workshop with some anxiety around internet, times, unsure what to expect and being the first of its kind.
Shabir Moosa, shared what and who AfroPHC was all about. Champion Nyoni talked on the Myers Briggs Type Indicator (MBTI). After the first hour the session broke into two rounds of different group discussions of 15 minutes each with introductions and reflecting on MBTI. Prosper Tumusiime of WHO AFRO welcomed the session between the group discussions. He mentioned several key global documents, including the Astana Declaration, the political declarations on UHC and SDG, and African declarations for financing. He bemoaned the lack of progress in Africa and called for acceleration of UHC especially for good acceptable quality PHC. Health systems were a priority, guided by the Regional Committee Framework for UHC/SDGs, documents strengthening the DHS and the UHC Flagship. He requested a whole society approach and welcomed efforts of AfroPHC in building teamwork.
The initial group feedback shared by participants was that this exciting meeting was very interactive with considerable value-added. Feedback on the MBTI was that it was an interesting opener and conversation starter. MBTI was seen as a very useful tool in teamwork. A closing remark was that the breakup sessions were just great despite nervousness around the technical challenges.
DAY 2
The second session 4-7pm Central African time 10th September with ±100 participants was moderated by Bongi Sibanda. Participants were introduced more explicitly to Mentimeter. Participants shared their professions: a mix of family doctors, nurses and other disciplines. Most participants were from Southern Africa with participants feeling excited and energised. The agenda was exploring what the community expects from ambulatory PHC service delivery in Africa. There was a well-moderated panel discussion for one hour, including several leaders within AfroPHC. There was then discussion in small groups of 8-12. After regrouping participants were excited, inspired and encouraged. The feedback from all participants on “What does the community expect from ambulatory PHC service delivery in Africa” was mostly accessible, comprehensive quality care in partnership with communities. Group feedback was that the community expects holistic accessible, acceptable multidisciplinary team care (including community healthcare workers), public-private partnerships and referrals that are tailored to the needs of the community and in partnership with them. The feedback from participants on the way forward was that it needed to be based on Africa-specific, multidisciplinary and multisectoral collaborative networking and advocacy. Participants found the session interactive, value-adding and innovative.
DAY 3
The third session 4-7pm Central African time 11th September with ±100 participants was moderated by Shabir Moosa. Participants were introduced more explicitly to Zoom Rooms and Mentimeter. Participants were from South Africa, Nigeria, Kenya, Tanzania, Malawi, Eswatini, Zimbabawe, USA, Germany and Argentina. Most were family physicians, family nurse practitioners, nurses, occupational therapists and a range of other professions. There was a quiz to get familiar with Mentimeter. People expected to interact more, meet primary care leaders from across Africa, learn about PHC in other countries, collaborate interprofessionally and across AfroPHC, and take action on a way forward to improve PHC in Africa. They enjoyed the panel discussions, interactions and group conversations.
Before the group discussions feedback was requested on “Who should be part of the PHC team in African PHC Service?” Nurses, doctors, pharmacists, community health care workers, dentist, social workers, occupational therapists’ clinical officers, and an array of others featured. There was a moderated panel discussion with leaders from AfroPHC and then discussion in small groups of 8-12 for 45 minutes on “Who should be part of the PHC team in African PHC Service?”, “How should the PHC teamwork in ambulatory PHC service delivery in Africa?” It was felt that all healthcare professionals and other stakeholders (patients, community and leaders) need to be part of the PHC team in an interprofessional team-based approach. There was tension between leadership by doctors and nurses, although a predominance expected coordinated, collaborative and consultative interprofessional teamwork. On “What support does the PHC team need in ambulatory PHC service delivery in Africa?” participants felt that PHC needed to be advocated for and prioritized with political and financial support and policies, education and training, infrastructure, community support, public-private partnerships, stronger supervision and teambuilding.
In closing participants felt that the workshop was outstanding for being highly interactive, informative, collaborative and networking. Suggestions for improvement were to have more networking workshops and include community voices.
On how we “Build PHC teamwork in Africa” participants suggested collaborations, regular workshops, training especially on teamwork, policy advocacy, and stakeholder engagement. On how we “Advocate for appropriate PHC and UHC” participants suggested good leadership, engaging politicians, community and PHC workers with a mix of research and training. Participants also wanted AfroPHC to be more formalized as an organization, with a conference/workshop statement emerging.
On the way forward most felt that AfroPHC should be formalized in an organizational format of a mix of individual membership with supporting organisations, with various activities suggested for AfroPHC to embark on, especially training, research, leadership and communication.
Help fund a nursing education project

Primary healthcare is the backbone of all strong health systems and forms a critical part towards the achievement of Universal Health Coverage. Now more than ever before, primary care nurses particularly those working in rural and remote settings must be appropriately supported through robust education/clinical supervision to meet population health needs safely and effectively. I have been facilitating developments towards this work in Africa since 2014 both voluntarily and as part of my doctoral work. As part of my final Doctor of Nursing Practice Project, I am leading work on the development of an Afrocentric Family Nurse Practitioner to inform educational….more
AFREhealth News June 2020

We are well into the COVID-19 pandemic, and across Africa, there is a call to ease lockdown measures and restart the econo-my. However, it still falls to us as scientists, researchers, health care professionals, and leaders to keep up the message of physical distancing, use of masks and washing hands frequently.
Pandemics come without a rule book. We do not know how the disease will progress, as we are still understanding the virus, and effective therapies. In the interim however, we can continue to strengthen our work-force, and provide them with the tools to provide quality and effective care. AFREhealth has engaged in a series of ac-tivities to do just that. Webinars, publica-tions on websites and in scientific journals and even animations are being used. We can however, only build on this by having mem-bers share their experience and expertise. Write to us, either for the newsletter, or in the AFREhealth blog. Tel us what you need. Share with us your best practices. Share your frustrations and successes.
It is up to African researchers, scientists and healthcare workers, together with econo-mists and social scientists to define and re-spond to this challenge so that we can work for solutions for Africa ourselves and strengthen our systems for our people by understanding our local contexts.
This newsletter presents some of the COVID-19 work. It does present other activities as well. A reminder that though we are dealing with a pandemic, other activities and other diseases still still deserve our attention. Stay safe and healthy! …..
Look at AfroPHC webinar on education of team in African PHC
Look at AfroPHC webinar on community development in African PHC
AfroPHC Webinar 6pm (GMT) Tues 19th May 2020
Dear colleagues

The African Forum for Primary Health Care (AfroPHC) is the voice of the PC/PHC team and its supporters, sharing and supporting each other in advocating for PHC. We want you to join us.
Please register here for our fourth webinar on Tues 19th May 2020 at 6 pm Ghana, 7 pm Nigeria, 8 pm SA, 9 pm Kenya.
The webinar will include luminaries in Africa talking about education of the team in African PHC.
- Mr. Champion Nyoni, Coordinator of AfrIPEN
- Prof Abigail Kazembe, Vice President of AFREhealth
- Representative of PRIMAFAMED
They will share a bit of background on organisations in the field, their efforts in the space of Primary Health Care in Africa as well as their views on the AfroPHC process.
Please forward this to your friends and colleagues.
rgds, AfroPHC Core Team
AfroPHC Webinar 6pm (GMT) Tues 21st April 2020

Dear colleagues
The African Forum for Primary Health Care (AfroPHC) is the voice of the PC/PHC team and its supporters, sharing and supporting each other in advocating for PHC. We want you to join us.
Please register here for our third webinar on Tues 21st April 2020 at 6pm Ghana, 7pm Nigeria, 8pm SA, 9pm Kenya.
The webinar will include luminaries in Africa talking about public health and community health workers in African PHC.
- Dr. George Kimathi, Senior Manager from Amref
- Prof. Godwin Aja, African Region of Towards Unity for Health
They will share a bit of background on organisations in the field, their efforts in the space of Primary Health Care in Africa as well as their views on the AfroPHC process.
Please forward this to your friends and colleagues.
rgds, AfroPHC Core Team
Look at AfroPHC webinar on family doctors and clinical officers in African PHC
Joburg PHC Plan for COVID-19
Johannesburg Health District’s Department of Family Medicine has developed a plan for the COVID-19 outbreak. Our concern is to protect patients AND you, as healthcare workers on the frontline.

The intervention is focused on three areas: community, facility and sub-district/district.
- Community: the key elements of the community response by facilities are to ensure community stakeholder involvement, deploy CHWs into the community and ensure a clear consistent message.
- Facilities: the key elements of the facility response is to set up a triage area at the facility gate to sort/screen/prioritise patients with flu symptoms, set up a temporary chest clinic to manage patients with flu symptoms, ensure strong protection of staff and management systems in this temporary chest clinic and have a strong overall approach by facility management.
- District: The key elements of the sub-district/district response are to ensure availability of equipment/staff/consumables for the overall response, ensure clinical governance at facility level, support overall communication and explore expanded services and contingencies.
The details are spelled out in the documents below.
COVID-19 Plan Jhb Health District 2020-03-19
COVID-19 Plan Jhb Health District 2020-03-19 APP Incident Management Team Organogram
WHO-WONCA Africa-AfroPHC Webinar on COVID-19 on 20th March 2020
WHO (Global and AFRO), WONCA Africa and AfroPHC are planning a weekly webinar on COVID-19 to get an update on the situation, explore preparedness in Africa and to respond to questions. This will be at 1pm Central European Time on Fridays with the first webinar this Friday, 20th March. Each webinar will focus on different parts and countries in Africa. The focus this Friday is Anglophone Africa. It will be Francophone Africa next week. We will elaborate the focus for each weeks webinar here as we proceed. Please circulate the link to this news post to everyone in primary care in Africa. We really hope to reach to all family doctors and PHC team members on the frontline, to support each other and ensure their voice is heard at the highest level.
Register for the first webinar: https://who.zoom.us/webinar/register/WN_5K4o4CiARvKARgriYI37vw
After registering, you will receive a confirmation email containing information about joining the webinar.

AfroPHC Webinar 6pm (GMT) Tues 17th March 2020

Dear colleagues
The African Forum for Primary Health Care (AfroPHC) is the voice of the PC/PHC team and its supporters, sharing and supporting each other in advocating for PHC. We want you to join us. We are having a series of webinars in a work up to the AfroPHC Conference 19-21 June 2020. Register for it!
Please register here for our second webinar on Tues 17th March 2020 at 6pm Ghana, 7pm Nigeria, 8pm SA, 9pm Kenya.
The webinar will include luminaries from family medicine talking about family doctors, associate clinicians and African PHC.
- Dan Abubakar, President-elect of WONCA Africa
- David Lusale, President of African Network of Associate Clinicians
- Albert Taiti, President-elect of African Network of Associate Clinicians
- Joy Mugambi, Secretary of WONCA Africa
- Zuki Tshabalala, Chair of Professional Association of Clinical Associates South Africa (PACASA)
They will share a bit of background on organisations in the field, their efforts in the space of Primary Health Care in Africa as well as their views on the AfroPHC process.
Please forward this to your friends and colleagues.
rgds, AfroPHC Core Team
AfroPHC Webinar 6pm (GMT) Tues 18th Feb 2020

Dear colleagues
The African Forum for Primary Health Care (AfroPHC) is the voice of the PC/PHC team and its supporters, sharing and supporting each other in advocating for PHC. We want you to join us. We are having a series of webinars in a work up to the AfroPHC Conference 19-21 June 2020. Register for it!
Please register here for our first webinar at 6pm (GMT) on Tues 18th February 2020.
The webinar will include luminaries from the nursing discipline talking about nurses and African PHC.
- Thembeka Gwagwa, 2nd Vice President of the International Council of Nurses (ICN).
- Bongi Sibanda, Coordinator of Anglophone Africa Advanced Practice Nurse Coalition Project (AAAPNC)
- Judy Khanyola, African Representative for Nursing Now
- Mwansa Nkowane, Consultant and ex-WHO AFRO
They will share a bit of background on organisations in the field, their efforts in the space of Primary Health Care in Africa as well as their views on the AfroPHC process.
Please forward this to your friends and colleagues.
rgds, AfroPHC Core Team
AfroPHC Conference
AfroPHC is planning a 3-day Launch Conference 19th – 21st June 2020 at the Faculty of Health Sciences, University of Witwatersrand, Johannesburg, South Africa. We hope to develop AfroPHC as the voice of the PC/PHC team and its supporters, sharing and supporting each other in advocating for PHC and a strong team-based approach to delivery.
There will be an Advanced Practice Africa Region Symposium on the 18th of June 2020 at the same venue. This will explore the development of Advanced Nurse Practice in Africa.
Primafamed, an African network for family medicine education/research in over 25 countries, will also have its annual meeting on the 17th June 2020 at the same venue. This usually explores family doctor education and research but will focus on team issues in this meeting.
Various leaders in PHC across Africa will be there: family doctors from WONCA Africa, clinical officers from the African Network of Associate Clinicians, family nurse practitioners from the Association of African Advanced Nurse Practitioners, nurse leaders from the International Council of Nurses, public health practitioners from the African region of Towards Unity for Health, health educators/researchers from AfreHealth, multidisciplinary team members from AfriPEN, community health worker/community leaders from AMREF and a variety of other key stakeholders. We are expecting key people from WHO Global, WHO AFRO and World Bank to be there.
The likely cost for teas/lunches will be $25 per person per day for African delegates and $50 per person for non-African delegates. Payment will be by Paypal.
The Holiday Inn Johannesburg Sunnyside Park Hotel is a walk away.
- Single Occupancy rate R1225.00 Bed and Breakfast per room per night
- Single Occupancy rate R1435.00 Dinner, Bed and Breakfast per room per night
There are many hotels in the vicinity and getting to Wits is easy with Uber.
Registration and more details will be forthcoming as we proceed.
#WoncaAfrica 06 November 2017
WHO QualityRights: transforming mental health services
Below are extracts from a new free-access article in The Lancet Psychiatry:
A movement to profoundly transform the way mental health care is delivered and to change attitudes towards people with psychosocial, intellectual, and cognitive disabilities is gaining momentum globally.
The Convention on the Rights of Persons with Disabilities (CRPD), which came into effect in 2008, clearly shows that changing attitudes towards — and practices — in mental health care is not only a necessity, but also an obligation under international human rights law…
Through [The QualityRights initiative] WHO is working to improve the quality of care provided by mental health services and promote the human rights of people with psychosocial, intellectual, and cognitive disabilities…
One of the most recent developments of the QualityRights initiative has been the publication of a set of 15 training and guidance modules. These modules help to build capacity among multiple stakeholders to change attitudes and practices in services and the community, and to create new services—including peer support—and strengthen civil society and advocacy efforts. These training modules have been developed in collaboration with more than 100 national and international actors including: disabled people’s organisations; non-governmental organisations; people with lived experience; family, care partners, and professionals working in mental health or related areas; human rights activists; lawyers; and others.
To support the transformation of mental health services, WHO QualityRights is currently developing a best practice guide. This guide will identify, describe and provide evaluation data for good, promising, and emerging community-based mental health and related support and services that are responsive to people’s needs, promote recovery, and are in line with international human rights standards…
CITATION: WHO QualityRights: transforming mental health services
Michelle Funk, Natalie Drew
Lancet Psychiatry, Volume 4, No. 11, p826–827, November 2017
DOI: http://dx.doi.org/10.1016/S2215-0366(17)30271-7
http://thelancet.com/journals/lanpsy/article/PIIS2215-0366(17)30271-7/fulltext?dgcid=etoc-edschoice_email_Nov
—
Best wishes, Neil
Let’s build a future where people are no longer dying for lack of healthcare information – Join HIFA: www.hifa.org
Dear HIFA group
I would just like to share with you the September 2017 issue of the Movement for Global Mental Health (MGMH) newsletter: http://sh1.sendinblue.com/nbc011z94c.html?t=1507120945. The October 2017 issue will be sent out by 1 November 2017. Should you wish to subscribe to the newsletter, please click on this link and enter your email address: https://my.sendinblue.com/users/subscribe/js_id/2oshf/id/1/email/demo@email.com
The Movement for Global Mental Health (www.globalmentalhealth.org) and the SA Federation for Mental Health (www.safmh.org) will be hosting the 5th Global Mental Health Summit in Johannesburg, South Africa from 8-9 February 2018. There are still spaces available and you can register now: http://www.globalmentalhealth.org/5th-global-mental-health-summit-2018-1
The panels of the Summit will focus on these themes:
· Persons with Lived Experience – the key partners in mental health and sustainable development
· Value of research to advance the social movement – the role of persons with lived experience in research
· Overcoming poverty through quality education and decent work and economic growth
· Changing the culture around mental health, mental disorders and emotional wellbeing
· Getting “creative and innovative” to achieve recovery and mental wellbeing
· Infants, toddlers and young children – affording them mental health and wellbeing
· Empowering the youth to play a role in achieving the SDGs
· Not forgetting the vulnerable groups
· Deinstitutionalisation and community integration – a human right
· Civil society’s role in achieving the SDGs
· Social movements giving a voice to persons with psychosocial and intellectual disabilities.
The information brochure and registration form is available at: http://www.globalmentalhealth.org/sites/default/files/5th%20Global%20Mental%20Health%20Summit%20INFO_1.pdf
Thank you
Kind regards,
Charlene Sunkel
Programme Manager: Advocacy & Development
SA Federation for Mental Health
T: +27 (0)11 781 1852
F: +27 (0) 86 558 6909
charlene@safmh.org
www.safmh.org
000-238 NPO / PBO 18/11/13/3099
Principal Coordinator: Movement for Global Mental Health
Apps to help the visually impaired access information: ‘Be My Eyes’
Dear Colleagues,
Today I came across this short video article from the BBC about a free app called ‘Be My Eyes’. Basically, it links a visually impaired person with a sighted volunteer in order by smartphone to help the former with a problem that they have.
http://www.bbc.co.uk/news/av/magazine-39056979/an-app-to-help-blind-people-to-see
A quick browse of the Be My Eyes website (http://bemyeyes.com/what-is-be-my-eyes/) and social media content gives some examples of the help that’s possible e.g.:
– read expiry dates on food
– read instructions
– help with a technical problem
– describe pictures/paintings
Immediately I thought of all sorts of health / health-information related issues that might be feasible, especially for the developing world e.g.
– read expiry dates on medicines
– read instructions on how to take medicines
– help use a piece of medical equipment
– describe what a boil or rash looks like before going to a doctor
However, the site suggests the app is NOT used for the following (among other things):
– Anything that can put your health in danger
– Identifying or taking medicine
– Any health related issues
I understand their concern/caution; nevertheless it made me wonder if there are other similar aids out there, aside from readers, for people with various disabilities? Meanwhile, there may be members who are aware of common problems faced by visually impaired caregivers and others? Maybe there are members who are developing aids?
Incidentally, I came across this link from the European Blind Union (EBU) on “Making information accessible for all” that may interest people producing (health) information that they want to be ‘accessible’:
http://www.euroblind.org/resources/guidelines/nr/88#How_do_blind_and_partially_sighted_people_read
Best wishes
Julie
HIFA profile: Julie N Reza is a writer, editor and consultant specialising in global healthcare and related fields (www.globalbiomedia.com). She predominantly works with NGOs and not-for-profit organisations. Previously she was the senior science editor at TDR, based at WHO in Geneva; prior to this she worked at the Wellcome Trust, UK, leading educational projects on international health topics including trypanosomiasis and trachoma. She has a PhD in immunology and a specialist degree in science communication. She also has several years research and postgraduate teaching experience. She is a member of the HIFA Steering Group and HIFA Social medica working group.
http://www.hifa.org/people/steering-group
http://www.hifa.org/people/social-media
http://www.hifa.org/support/members/julie
Email: naimareza AT hotmail.com
Dear Julie,
Thank you so much for this valuable information.
I am a Tanzanian, became blind at the age of 50 years, and I am currently making use of screen readers to access information.
We from developing countries still need much assistance from developed world, we face a lot of challenges such as financial constraints, technical know how etc.
I have been very much impressed by the way this app (Be My Eyes) works and by this e-mail I would like to welcome anybody or organization to work with our organization in Tanzania so as to enable the visually impaired Tanzanians manages their daily living independently.
I’m a chairman of Computers For The Blind (CFTBT), a no-government organization registered in Tanzania and it is also a non-profit organization being run by people with blindness and visual impairment.
The main objective of our organization is to train blind and partial sighted persons to access information through computer application.
Welcome all,
Clement Y.Ndahani: CFTBT Chairman
E-mail: clement.ndahani@out.ac.tz
HIFA profile: Clement Yoramu Ndahani is a Technologist at The Open University of Tanzania. Professional interests: Social work. clement.ndahani AT out.ac.tz
Dear Clement,
Yours is exactly the type of response I was hoping to see.
I would imagine that there are many app developers – in high, medium and low-income countries – who would like to build apps that will help people with disabilities. But they may be unaware of the particular issues that you face in Tanzania and similar countries. I hope that through HIFA these messages find the right people and that some useful collaborations develop.
Incidentally, here in the UK, and I believe in many other countries, there are ‘hackathons’, in which developers/scientists come up with innovative solutions to a variety of problems. I notice that in Tanzania you have just had one such event http://daressalaam.sciencehackday.org/about-dar/ (Science Hack Day Dar es Salaam). I wonder if one approach would be to take part in or even host such an event?
On a slightly different note, the ‘Be My Eyes’ app also made me wonder if it would be adaptable for use by (a) groups with low literacy (a kind of ‘Be My Reader’) and (b) people with different languages/dialects (a kind of ‘Be My Translator’).
I wish you well with your endeavours.
Best wishes
Julie
HIFA profile: Julie N Reza is is a writer, editor and consultant specialising in global healthcare and related fields (www.globalbiomedia.com). She predominantly works with NGOs and not-for-profit organisations. Previously she was the senior science editor at TDR, based at WHO in Geneva; prior to this she worked at the Wellcome Trust, UK, leading educational projects on international health topics including trypanosomiasis and trachoma. She has a PhD in immunology and a specialist degree in science communication. She also has several years research and postgraduate teaching experience. She is a member of the HIFA Steering Group and HIFA Social medica working group.
http://www.hifa.org/people/steering-group
http://www.hifa.org/people/social-media
http://www.hifa.org/support/members/julie
Email: naimareza AT hotmail.com
Dear Julie
I am a Nigerian and a Librarian. How do I get access to the app. [*see note below] I work with students with special needs and there are about One hundred and twenty-three visual challenged students among them.
HIFA profile: Ngozi Eunice Osadebe is a librarian at the University of Nigeria, Nsukka. Professional interests: Enhancing access to higher education for people with disability, Technology Assisted Learning. She is a member of the HIFA working group on Library and Information Services.
http://www.hifa.org/projects/library-and-information-services
http://www.hifa.org/support/members/ngozi-eunice
ngozi.osadebe AT unn.edu.ng
[*Note from HIFA moderator (Neil PW): Please see the Be My Eyes website http://bemyeyes.com/what-is-be-my-eyes/ ]