As a beacon for frontline health workers devoted to Primary Health Care (PHC) service delivery and the realization of Universal Health Coverage (UHC) in Africa, we are excited to announce the launch of the AfroPHC Policy Framework titled “Building the PHC Team for UHC in Africa.”
Event Details:
- Date: October 12, 2023
- Time: 12:00 Greenwich Mean Time
- Platform: Zoom Webinar
- Registration Link: AfroPHC Policy Framework Launch Registration
Why Attend?
- Deep Dive into the AfroPHC Policy Framework: Gain insights into our comprehensive guideline crafted to build a resilient PHC team pivotal for driving UHC in Africa.
- Engage in Rich Discussions: Partake in an interactive webinar, group deliberations, and a Q&A session to exchange experiences, perspectives, and best practices.
- Drive Recommendations: Be part of a collective voice shaping the future of PHC teams, financing models, and effective PHC policy implementations.
- Collaborate: Join stakeholders, policymakers, healthcare professionals, and communities in a unified mission to bolster PHC for UHC in Africa.
Event Structure:
- Welcome (10 mins): Introduction to the AfroPHC Policy Framework.
- Keynote (10 mins): Emphasizing the role of a robust PHC workforce for UHC.
- Thematic Presentations (80 mins): Covering topics like multidisciplinary teams, community health workers, PHC financing models, and PHC Implementation Country successes and lessons.
- Q&A Session (20 mins): Address audience queries.
- Group Discussions (45 mins): Theme-based dialogues to drive actionable insights.
- Plenary (60 mins): A summary of group findings and a moderated cross-theme exploration.
RSVP: register in advance for the webinar. Post registration, you will receive a confirmation email with further joining details. Please share this within your networks nad with your members.
In a world where patients and health workers often get lost in bureaucracy, our vision stands clear: an empowered, people-centric PHC team aptly equipped for Africa’s unique needs. We count on your invaluable participation to bring this vision closer to reality.
Meet Our Speakers

Dr. Jeff Markuns is a practicing family doctor and faculty member at Boston University, and currently the President for the North America Region of the World Organization of Family Doctors (WONCA). Most recently, Jeff was the Executive Director of the Primary Health Care Performance Initiative (PHCPI), a partnership between the Bill & Melinda Gates Foundation, the World Bank Group, UNICEF, the Global Fund and the World Health Organization with Ariadne Labs and Results for Development (R4D) as technical partners, all focused on better primary health care measurement for improvement in low and middle income countries. Jeff has particular expertise in education as the current and founding Director of the Masters program in Health Professions Education at Boston University. Jeff’s earlier clinical work has included both outpatient and inpatient services, including 20 years of labor and delivery, his teaching experience included his work as an Assistant Program Director for BU’s residency in Family Medicine, and his operational experience included leading one of BU’s primary Family Medicine clinical units in an affiliated community health center. As the Executive Director of the Global Health Collaborative in the Department of Family Medicine, Jeff’s deep experience with frontline primary health care and the human resource capacity-building necessary to support its success has led to successful long-term vertically and horizontally-integrated development efforts to promote primary health care system strengthening and workforce development, supporting programs throughout southeast Asia and in Lesotho in southern Africa.

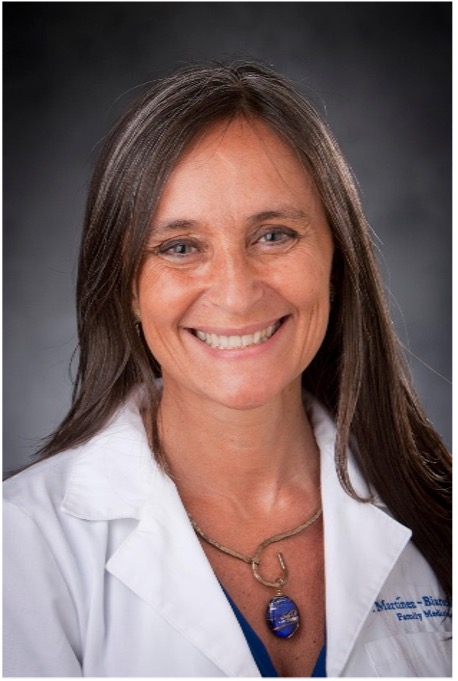
Dr. Viviana Martinez-Bianchi is a family doctor, a fellow of the American Academy of Family Physicians, an Associate Professor, and the Director for Health Equity at Duke University’s Department of Family Medicine and Community Health, in North Carolina, USA. She served as Executive Member-at-Large of the World Organization of Family Doctors (WONCA) and WONCA liaison to the World Health Organization from 2016-2021, she is a member of the WONCA Rural Council, and has chaired WONCA’s Organizational Equity committee. She has been a member of the AfroPHC Advisory since its inception. She serves in multiple organizations, boards, taskforces and advisories addressing care for marginalized populations.

Dr. Faraz Khalid is currently a Research and Innovation Officer at Special Program for Primary Health Care at WHO Headquarters, and before this role, he was responsible for coordination for Universal Health Coverage reforms at the WHO’s Eastern Mediterranean Regional Office.
He has taken on multiple roles in the low- and middle-income countries health systems in the last seventeen years. He started his career as a medical doctor, transitioned to a program manager of an award winning innovative mhealth enabled social health protection program in Pakistan, has worked as health systems and financing consultant with World Health Organization, UNICEF, Asian Development Bank, and USAID.
Following his medical training, he completed his PhD in Global Health Policy and Management from Tulane School of Public Health and Tropical Medicine, USA and did Master’s in public health from London School of Hygiene and Tropical Medicine.

Dr. Salim Ali Hussein is a Public Health Practitioner in the Ministry of Health, heading Primary Health Care, in the Ministry of Health, Kenya since July 2019. Passionate in Health System strengthening.
Previously held positions; head of Department of Health Promotion, Division of Community Health and has been a District Medical Officer In Charge of Marsabit District and Makindu Sub District. He holds an MSc Public Health System Management and Application from Kenyatta University and MB ChB from University of Nairobi. I have been trained on Social Innovation and system Change at University of Cape Town, leading high performing healthcare organizations (LeHHO) at Strathmore University, Strategic Leadership Development Programme at Kenya School of Government, in Information, Education & Communication in Health at Okinawa International Centre, Japan, and in Executive Hospital Management at United State International University, Nairobi.

Dr Kalangwa Kalangwa is a Zambian medical doctor working for the Ministry of Health Headquarters as Assistant Director Health Promotion and Community Health in the department of Public Health and Research. He is also the spokesperson for the Ministry of Health. He has a special interest in solving health challenges using a public health approach. He has over 8 years experience in clinical medicine and public health. He holds a bachelor of science in Human Biology, a bachelor of Science in Medicine and Surgery and a masters degree in Epidemiology and Biostatistics, all obtained from the University of Zambia. He is currently perusing an MBA in Healthcare Management at UNICAF
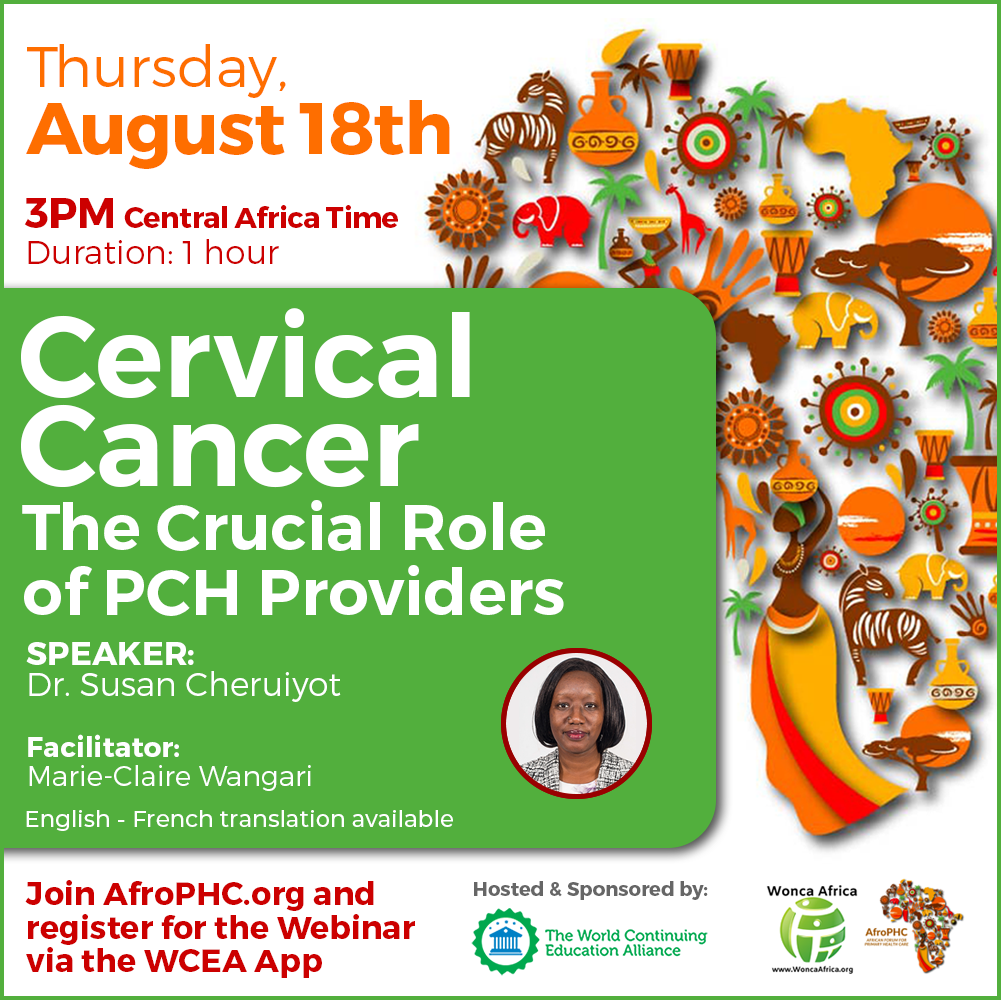
The Virtual Workshops
The policy was constructed by over 500 members from over 20 African countries through virtual workshops since 2020. The workshops occurred on every third Tuesday of every month, 1-4 pm Central African Time, and the aim was to help build a shared perspective amongst PHC team members across Africa. All workshops were in the format of a moderated discussion with panellists and then group discussion and feedback. These workshops were accredited for continuing medical education (CME)/continuing professional development (CPD) across many African countries. They also had English/French/Portuguese translators available.
Final Policy Framework Workshop in Johannesburg, South Africa
In October 2022, AfroPHC was able to host an in-person meeting in Johannesburg, South Africa. The purpose of this meeting was to finalise the policy paper, and the call to action for PHC across the African continent. About 35 members of the AfroPHC Executive and Advisory Board convened, together with other key stakeholders and experts, as the first in-person meeting of AfroPHC.
The Executive Summary
As the largest grassroots African institution specifically dedicated to advocating for frontline health workers who are committed to PHC service delivery and universal health coverage (UHC), we call on all stakeholders across Africa to build and empower effective PHC teams to achieve high quality PHC and UHC in Africa.
Our experience of primary health care (PHC) is of patients who are treated as numbers in a queue, with poor comprehensiveness, continuity, and coordination. Health workers are also treated like numbers in a bureaucracy that fragments and undermines training and service for integrated care around patient and population needs.
Our vision for PHC and UHC is a PHC team with skills mix appropriate to Africa, including family doctors, family nurse practitioners, clinical officers, community health workers and others that are empowered to take care of an empaneled population in high-quality people centred PHC.
Africa, please heed to the call of your health professionals.
Currently, the PHC system in Africa faces many new challenges AND opportunities. To date, human resources for health in PHC are grossly insufficient in number, often inefficiently and inequitably distributed, lacking adequate training for delivering fully responsive and comprehensive frontline care, and are treated inequitably within the health system. Projections for the African health workforce suggest this will worsen over the next five years. There has been a lack of solidarity among key role players in healthcare to create adequate PHC funding in Africa. Resources do not appropriately or adequately reach the frontline PHC service platform due to outdated service delivery and payment models. However, there are opportunities that leaders can capitalize on: global PHC milestones, increasing political will for investment in PHC, and proven mechanisms for achieving a stronger workforce such as the professionalization and scaling up of community health workers, clinical role-sharing, and the integration of family doctors, advanced practice nurse practitioners and allied health professionals into PHC.
We call on African leaders and global stakeholders to develop and implement a regional forward-looking plan to:
1)Build robust PHC SYSTEMS.
This must be based on a high quality bio-psycho-social-spiritual approach for PHC that is comprehensive, coordinated and integrated person- family- and community-centred. It must integrate PHC priorities and Health in All Policies. It must be based on empanelling of defined populations to a specific PHC team using community oriented primary care. It must be supported by interoperable e-Health and a strong District Health System to coordinate public and private providers.
2)Educate, recruit and maintain a sufficient frontline PHC WORKFORCE.
This must include a complete workforce of locally trained family doctors, nurses, advanced practitioners, pharmacists, professionalized community health workers and others sufficient to deliver high quality PHC. This workforce must involve role-sharing with supportive supervision; distributed leadership; clinical governance by accountable clinicians; and an integrated human resources development and management plan suitable to PHC.
3)Support PHC with FINANCES.
There must be political and sustained funding action that considers PHC as an investment; a fight for global solidarity action on PHC funding pools; and better management of PHC across Africa with strategic purchasing and payment reforms using blended capitation.
This can all come together easily in a simple nationally-defined PHC contract using risk-adjusted blended capitation payment to decentralised PHC teams empanelled to enrolled populations, coordinated by the district health services to provide services to the full population, and easily administered at national or sub-national level for empowered public and private providers.
As the African Forum for Primary Health Care, we call on Africa to commit to making this plan a reality and building effective PHC teams for UHC in Africa. We commit to mobilising PHC workers across Africa to create PHC teams around empanelled populations as sentinel sites across Africa to share best practice and to show evidence of how effective we can be at both practice and population level if we are empowered to deliver quality PHC as a team.
The AfroPHC Call to Africa: Join AfroPHC and build effective primary health care teams for universal health coverage in Africa
In opening we call on Africa
- To pay heed to the call of its health professionals for PHC and UHC in Africa.
- To seize opportunities to overcome African challenges for PHC and UHC in Africa.
- To embrace the World Health Report of 2008 and Astana Declaration of 2018 by prioritizing integrated, resilient, person-centred and high quality PHC within UHC, re-organising UHC around PHC service delivery, integrating public health with primary care, and bringing private PHC providers into a regulated PHC system for UHC in Africa.
In terms of PHC Systems we call on Africa
- To embrace the disciplines of family medicine and generalist PHC, with its bio-psycho-social-spiritual approach to care, to achieve PHC and UHC in Africa by 2023 that is personalised, comprehensive, continuous, and coordinated, in line with global standards.
- To embrace primary care, defined by WHO as an essential level of care, that needs to be responsive, person- family- and community-centred and covers the full spectrum of care within the paradigm of OneHealth for PHC and UHC in Africa by 2023.
- To integrate priority programmes (communicable diseases, non-communicable diseases, mother-woman-child health, violence-trauma, mental health etc.) into PHC in a diagonal manner that both supports these vertical priorities as well as supporting horizontal integration by PHC teams around patient and population for UHC in Africa by 2033.
- To strengthen rehabilitation and palliation in PHC by 2033 with decentralised and well-funded community rehabilitation and palliation services, where teams with an appropriate mix of skills and professional supervision are linked to multiple community practices for accountable care.
- To integrate oral health into PHC by 2033 with team-based service delivery models that includes appropriate role- and task-sharing with a range of oral health care practitioners and dentist support and supervision and that are linked to multiple community practices for accountable care.
- To strengthen access to medicines and investigations with greater embrace of pharmacy professionals and point-of care technology at PHC level to achieve PHC for UHC in Africa by 2033.
- To strengthen coordination of PHC referrals to hospitals with the placement of postgraduate-trained family doctors in PHC teams by 2033 to achieve UHC in Africa.
- To prioritise PHC as the foundation for UHC: making “Health in All Policies” an integrating and developmental public health approach to decentralised government, and strengthening PHC teams with local linkages to other sectors affecting social determinants of health by 2023 to deliver PHC and UHC in Africa.
- To strengthen the district health service to coordinate decentralised and empowered providers by 2033 and to ensure they deliver on agreed-upon results as they implement PHC and UHC in Africa.
- To embrace the strategy of empanelment of a defined population and linking them to a defined, fully staffed, and equipped PHC team and medical home by 2023 as a foundational step to achieving PHC and UHC in Africa.
- To embrace community-oriented primary care in community practices of 30 000 by 2033 and aspire to community practices of 10 000 for achieving PHC and UHC in Africa by 2043.
- To embrace the Blueprint for Rural Health and rural proof all health policies by 2023 to support rural and marginalised urban primary health care comprehensively, especially creating stepladder entry requirements for educational institutions and rural/marginalised urban student immersion for the full PHC team, to achieve PHC and UHC in Africa.
- To recognise the unique challenges of women in PHC and to explore innovative and sustainable interventions to overcome these for PHC and UHC in Africa
- To recognise the unique opportunities of youth in PHC and to explore innovative and sustainable interventions to address these for PHC and UHC in Africa.
- To embrace the variety of eHealth solutions for PHC by ensuring that sustainable national e-health strategies are supported by accessible infrastructure, interoperability and user-friendly designs that enable the PHC team and patients/populations to enhance quality and support new models of care in PHC and UHC in Africa.
- To engage communities and ensure social participation in advancing team-based PHC across Africa.
- To embrace the culture of quality and patient safety with strong teamwork, and to measure and monitor performance to achieve quality PHC and UHC in Africa.
- To develop and support practice and population research sites focussed on PHC across Africa and to expand the range of indicators that will assess the effectiveness of PHC teams empanelled to populations as a key service delivery reform
In terms of PHC Workforce we call on Africa
- To build a larger, better trained PHC workforce (integrating public and private providers) with more opportunities (educational, financial, and clinical) and greater resources (starting with structurally defining PHC services) to enable PHC and UHC.
- To acknowledge the burden on all cadres in PHC and to embrace trans professional collaboration with a mix of all health professionals using respectful, collaborative role sharing and supportive supervision for achieving PHC and UHC in Africa.
- To embrace distributed leadership practices, and education for it, among all PHC workers and managers to achieve PHC and UHC in Africa.
- To embrace the important role of medical, dental, nursing and other professions with post-graduate training for decentralised primary care settings to support clinical governance, coordinated care and efficient referrals to achieve PHC and UHC in Africa.
- To standardise, professionalise and decently remunerate community healthcare workers that are strongly integrated with the PHC team, and furthermore to aspire to a target of one CHW per thousand persons by 2043 to achieve PHC and UHC in Africa.
- To clarify and harmonise PHC workforce nomenclature for the different categories and disciplines in PHC, and to then embark on labour market analyses in PHC (including public and private) and specific PHC human resource for health (HRH) policies and strategic plans to scale up the PHC health workforce by 2033 to achieve PHC and UHC in Africa.
- To implement a robust educational and credentialing systems for developing a competent workforce dedicated to delivering comprehensive PHC services necessary to achieve UHC in Africa.
- To protect all PHC workers as a precious and vulnerable resource and to empower them to build quality and resilience as a team that works closely with communities to achieve PHC and UHC for Africa.
In terms of PHC Finances we call on Africa
- To regard health as an investment and to leverage political goodwill for action on PHC/UHC by defining PHC in budget terms, ringfencing the financing of PHC and committing to at least 2% of their GDP on PHC for UHC in Africa.
- To re-examine global social solidarity on PHC and strengthen contributions to PHC for UHC in Africa as a priority, starting with High-Income Countries increasing ‘donor aid’ to 2% of their health spend and ‘donor aid’ funds allocating 30% to an African Union funding pool for integrated PHC and UHC in Africa by 2033.
- To work towards better funded single pools for UHC funding, prioritising strategic purchasing for PHC with standard and transparent contracting of both public and private providers in empowered decentralised units of PHC for UHC in Africa by 2043.
- To embrace PHC teams paid by blended capitation models (including capitation, fee-for-service and performance payments) to achieve holistic and responsive PHC and UHC in Africa by 2043.
- To embark on simple nationally-defined PHC contracting to community practices for accountable care from both public and private service providers.
In closing,
We call on Africa to empower and build an effective PHC team to achieve PHC and UHC in Africa. We, as the African Forum for Primary Health Care (AfroPHC), commit to educating and empowering providers and their communities at the frontline to support this goal in any way we can, including
building AfroPHC Chapters at country level as a forum
for PHC and UHC in Africa.



















-1.png?width=1200&upscale=true&name=Banner_Afro%20(5)-1.png)
-1.png?width=1200&upscale=true&name=Banner_Afro%20(3)-1.png)



-1.png?width=1200&upscale=true&name=Banner_Afro%20(2)-1.png)


